What is hyponatremia?
Hyponatremia is a condition in which there is an excess of body water relative to body sodium1
Often defined as serum sodium concentration < 135 mEq/L
[Na+] < 135 mEq/L
Hyponatremia may be depletional, or dilutional2,3
- Depletional hyponatremia results from body electrolyte losses that are in excess of body water losses3
- Dilutional hyponatremia results from retained water and is often associated with an excessive secretion of vasopressin2,3
Hypotonic hyponatremia is classified into 3 main categories
These categories are based on the initial assessment of the patient's volume status, medical history, urine osmolality, and sodium concentration.1,3
The 3 main categories with their volume status are illustrated below.
| Hyponatremia Category |
Total Body Water | Total Body Sodium | Extracellular Fluid | Edema |
|---|---|---|---|---|
| Hypovolemic | Reduced | Reduced | Reduced | Absent |
| Euvolemic | Increased | Unchanged | Increased | Absent |
| Hypervolemic | Increased | Increased | Greatly Increased | Present |
The figure below provides a guide for classifying hyponatremia into categories.
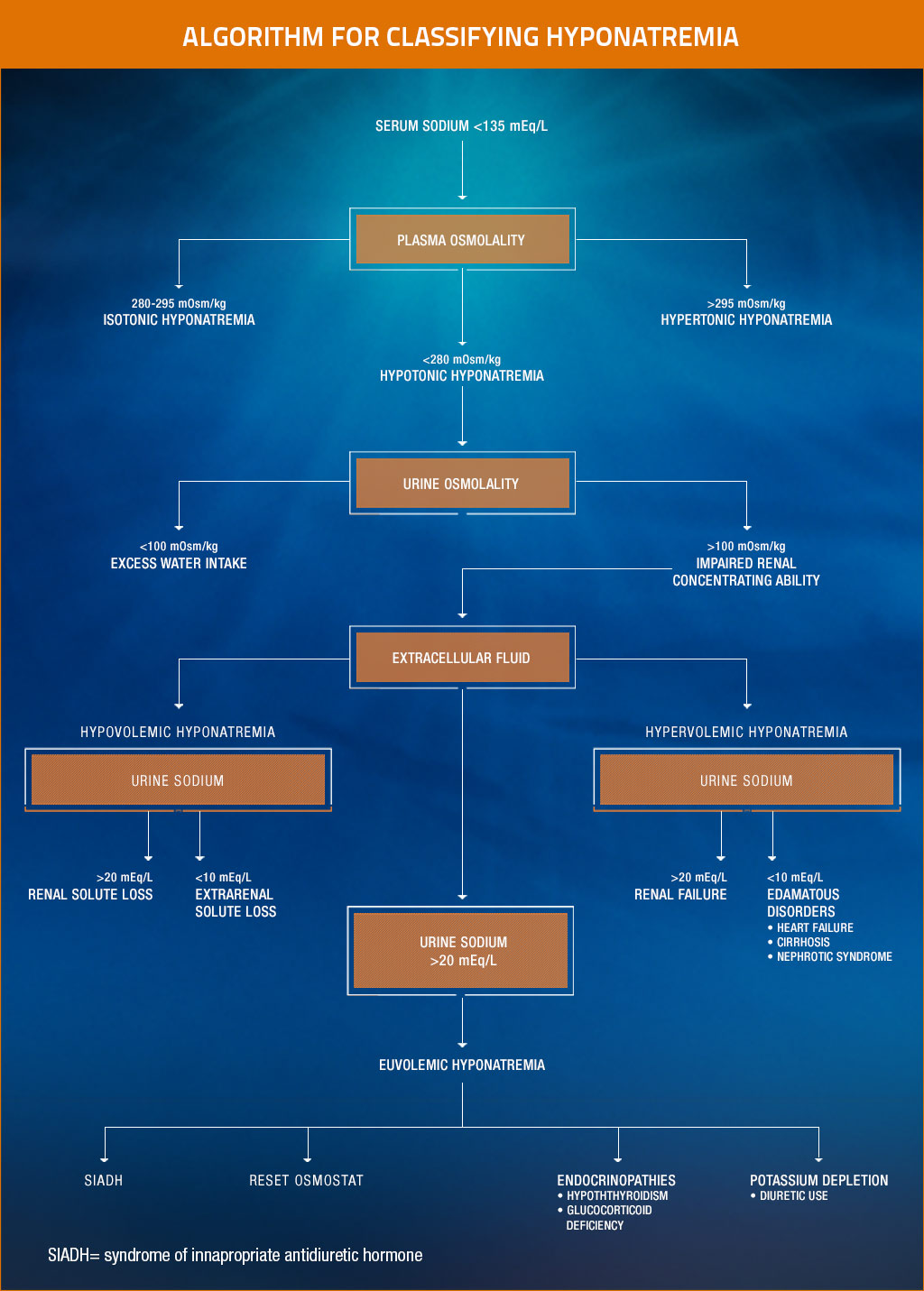
Based on assessment of volume status, medical history, and urine osmolality and sodium concentrations, hyponatremia can be classified as hypovolemic, euvolemic, or hypervolemic. Douglas I. Hyponatremia: why it matters, how it presents, how we can manage it. Cleve Clin J Med. 2006;73(suppl 3):S4-S12. Reprinted with permission. Copyright © 2006 Cleveland Clinic. All rights reserved.
Prevalence of Hyponatremia
In the United States, the estimated prevalence of hyponatremia ranges from 3.16 million to 6.07 million persons.5
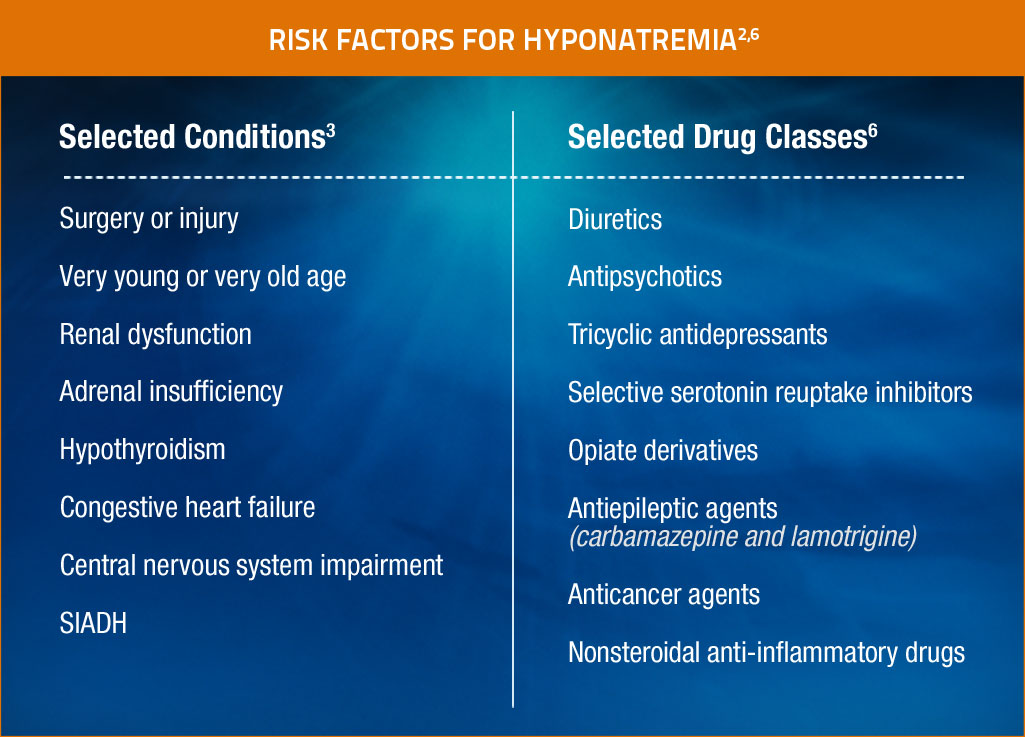
Risk Factors
Certain medical conditions and medications have the potential to increase the risk of hyponatremia.2,6
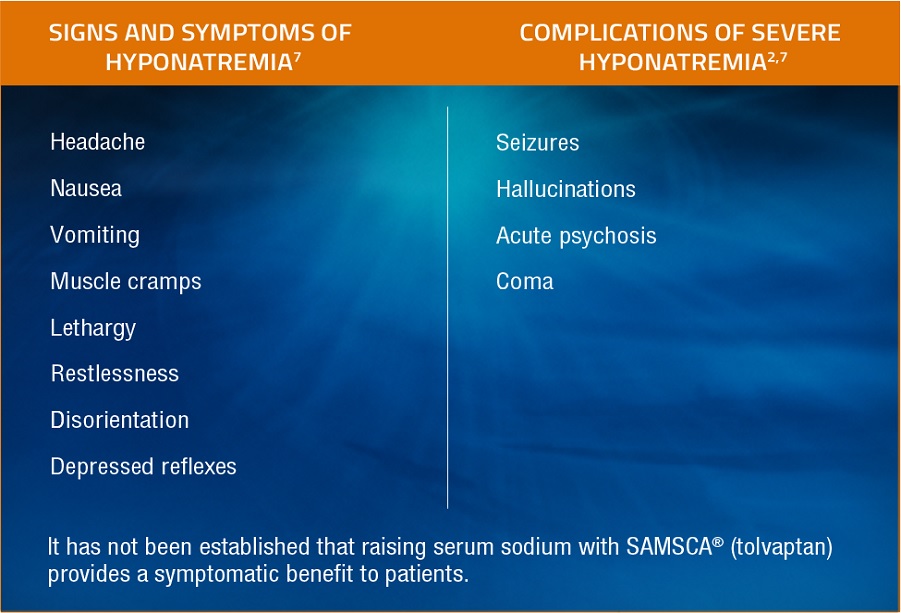
Signs & Symptoms
Patients who experience hyponatremia may exhibit clinical manifestations that are largely related to central nervous system dysfunction. Signs and symptoms are important to recognize.2,7

Review clinical cases about patients with hyponatremia in heart failure and hyponatremia in SIADH

See how SAMSCA works to promote free water clearance by direct antagonism of the renal V2-receptors.